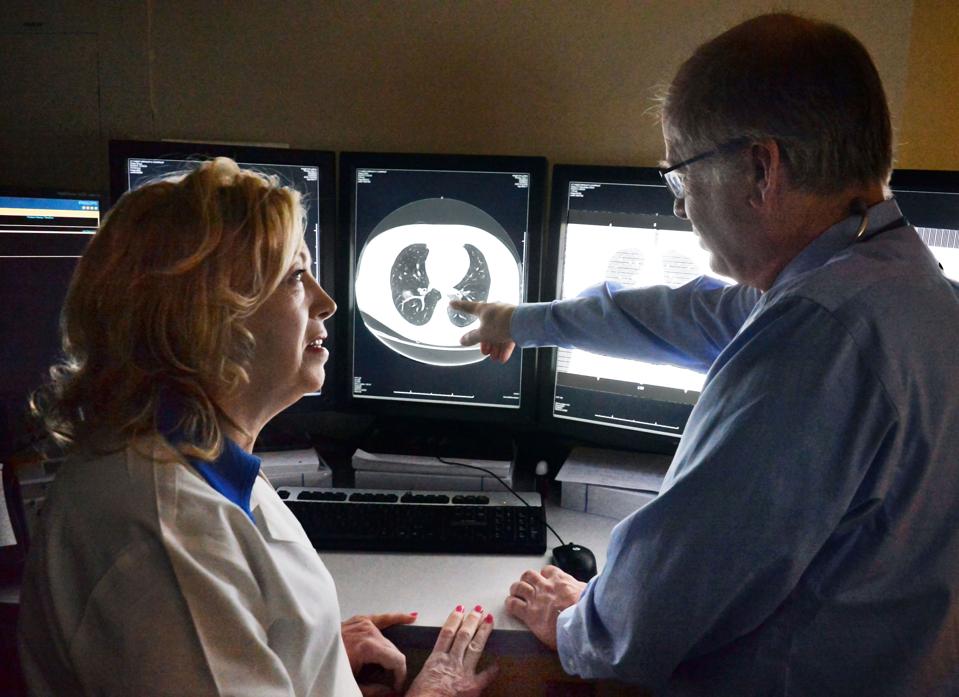
Division of Pulmonology and Critical Care nurse practitioner Jeanne Millett, left, and pulmonologist Dr. Thomas Smith review lung cancer screening scans at Albany Medical Center Friday Feb. 5, 2016 in Albany, NY. (Photo by John Carl D’Annibale /Albany Times Union via Getty Images)
Albany Times Union via Getty Ima
Lung cancer screening remains strikingly underused, with reported screening rates as low as 16% according to the American Lung Association. This means less than 1 in 5 individuals who are eligible to get a low-dose CT scan, the screening test for lung cancer, are actually …
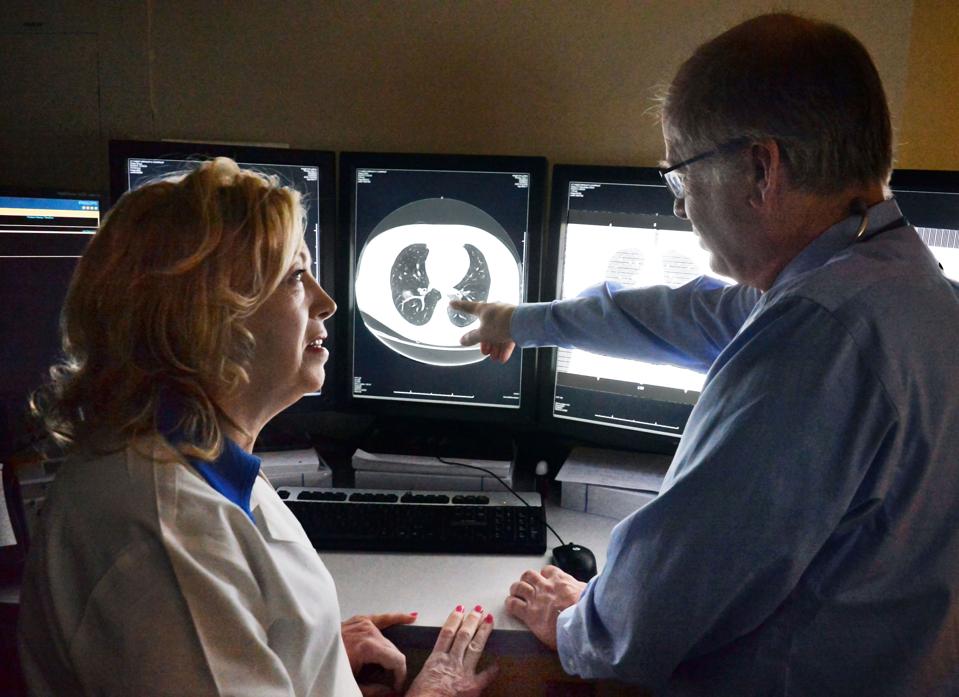
Division of Pulmonology and Critical Care nurse practitioner Jeanne Millett, left, and pulmonologist Dr. Thomas Smith review lung cancer screening scans at Albany Medical Center Friday Feb. 5, 2016 in Albany, NY. (Photo by John Carl D’Annibale /Albany Times Union via Getty Images)
Albany Times Union via Getty Ima
Lung cancer screening remains strikingly underused, with reported screening rates as low as 16% according to the American Lung Association. This means less than 1 in 5 individuals who are eligible to get a low-dose CT scan, the screening test for lung cancer, are actually getting the test. This statistic is worrisome since lung cancer is the leading cause of cancer death among both men and women.
According to the United States Preventive Services Task Force, individuals between the ages of 50-80, who have a 20 or more pack-year history of smoking and currently smoke or who have quit within the last 15 years should be screened annually for lung cancer with a low dose CT study. This type of study takes less than five minutes to perform, and involves special types of x-rays that take pictures of your lungs while you lie flat on a table. Research shows screening with this test reduces mortality by 20%. Despite the clear benefit, screening rates remain abysmal. Here are some reasons why.
Patient Factors
Awareness among patients remains a major bottleneck for screening. Many smokers or those who meet criteria to get screened are not even aware that lung cancer screening exists or do not know what a low dose CT scan of the chest is. A 2023 Early Detection Survey administered by Prevent Cancer Foundation revealed two in five respondents were unable to identify the accurate description of a lung cancer screening test.
Additional barriers include fear of a cancer diagnosis, stigma related to being labeled a smoker and concerns about radiation exposure from a CT scan. The study delivers about 1 to 4 millisieverts of radiation to the body, which is four to five times less than a normal CT chest would give. This amount of radiation is also equivalent to the amount of radiation one would get from background exposure in the environment for six months, exposure all humans naturally receive.
Physician Factors
Primary care doctors are the physicians that usually discuss the importance of screening tests with patients, whether to get them and risks and benefits associated with them. Research shows that less than 10% of physicians regularly discuss lung cancer screening with their patients, according to a study published in Cancer Epidemiology, Biomarkers & Prevention. Some physicians have reported uncertainty about eligibility rules, how to manage incidental nodules on chest x-rays and finding time to arrange shared-decision making communication with their patients.
MORE FOR YOU
In addition, although most low-dose screening studies are covered by Medicare, Medicaid and private insurance companies, the need for prior authorizations or even copays from some insurance providers can deter both physicians from recommending the study and also patients from making it to imaging centers to get screened.
USPSTF November Meeting Cancelled
The USPSTF, a scientific panel of national experts in preventive and evidence-based medicine, periodically provide recommendations for the American public on what screening tests should be performed for the American public based on age and risk factors. Their meeting that was slated to occur in November has been cancelled, which follows their July meeting that was also abruptly cancelled.
The downstream effect of such cancellations could result in delayed guideline updates, muddled public health messaging and uncertainty from patients and physicians about what tests will be covered by health insurers, since most insurers provide cost-free coverage for preventive services recommended by the USPSTF. The end result could mean less Americans get screened for the deadliest cancer, worsening health outcomes for cancer survival.
It is crystal clear that lung cancer screening saves lives. Consistent stewardship from the USPSTF in amplifying evidence-based guidelines coupled with physicians communicating the importance of the screening test will be necessary to ensure those that are eligible for the study get it. Bolstering education for patients and community outreach to address fear and stigma also must remain priorities to move the needle on improved lung cancer screening rates.